Article by Fundacia
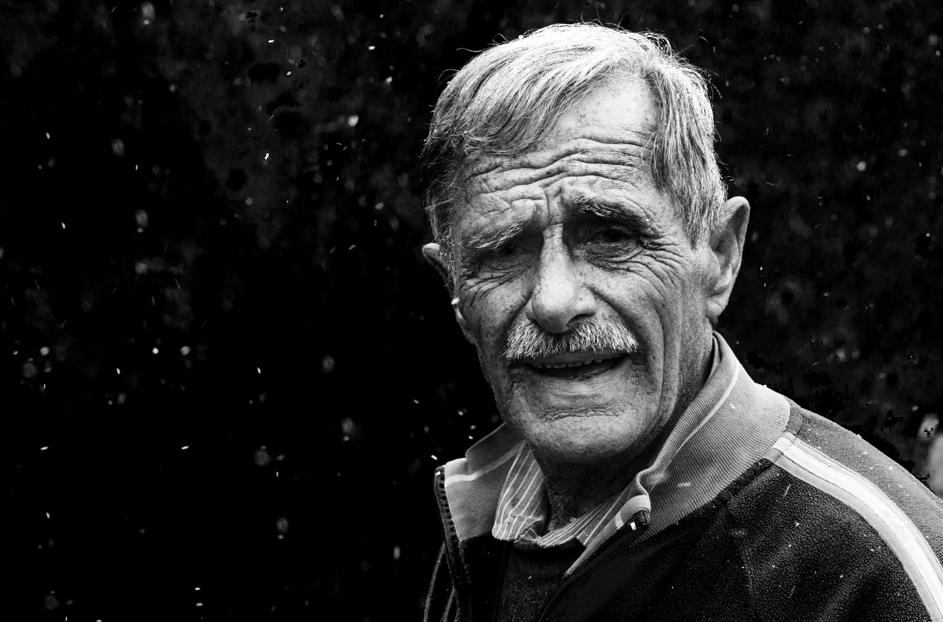
Depression in the elderly is common, but this does not mean it is normal. Only a small percentage of seniors use the help of a doctor. Older people often present symptoms of depression differently. Depression in the elderly is therefore often confused with the effects of other diseases and the drugs used to treat them.
Depression affects older people differently than younger people.
In the elderly, depression often accompanies other medical conditions and disabilities and lasts longer. Depression in the elderly is associated with a higher risk of heart disease and death from the disease. At the same time, depression reduces the elderly person’s ability to rehabilitate. Older people may not have obvious symptoms of depression. Instead, they can: feel tired, have trouble sleeping, be grumpy or irritable, feel confused, struggle to pay attention, not enjoy activities they used to, move more slowly, have a change in weight or appetite, feel hopeless, worthless, or guilty, experience aches and pains, have suicidal thoughts.
Using a series of standard questions, your primary care physician can check for depression, enabling better diagnosis and treatment.
Advanced age is often associated with the loss of social support systems due to the death of a spouse or sibling, retirement or relocation. Depression also increases the risk of suicide, especially for older men.
Factors that increase the risk of depression in the elderly include: being a woman, being single, unmarried, divorced or widowed, lack of social support, and stressful life events
Illnesses such as stroke, high blood pressure, diabetes, cancer, dementia and chronic pain, for example, further increase the risk of depression. In addition, the risk of depression is greater for older people who: have an injury (as a result of amputation, cancer surgery or a heart attack), are dependent on the help of others, need to stay in a hospital or need home health care, are unable to constructively cope with the fear of death, live alone, were to previous suicide attempts, experience chronic or severe pain, have already had depression, have recently lost a loved one, are abusing psychoactive substances.
What are the treatments for depression in the elderly?
Treatment of depression includes medicine, psychotherapy or counseling, electroconvulsive therapy, or other newer forms of brain stimulation (such as repetitive transcranial magnetic stimulation or rTMS). Sometimes a combination of these treatments can be used. The option your doctor may recommend depends, among other things, on the type and severity of your depression symptoms, your past therapies, and your overall health.
Most people with depression find support from family and friends, involvement in self-help and support groups, and psychotherapy. Psychotherapy is especially beneficial for those who have gone through severe life stresses (such as loss of friends and family, home relocation, and health problems) or who prefer not to take medications and have only mild to moderate symptoms. Many doctors recommend psychotherapy along with antidepressants.
What Problems Affect Treatment of Depression in Older Adults?
The fear of stigma associated with mental illness and psychiatric treatment is even stronger among the elderly. This can keep the elderly away from admitting that they are depressed. Older people and their families also can sometimes misidentify depression symptoms as “normal” responses to life stresses, loss or the aging process.
Moreover, depression can be expressed through physical ailments rather than traditional symptoms. This delays appropriate treatment. In addition, elderly people with depression may not report their depression because they mistakenly believe that there is no hope of help.
Older adults may also be reluctant to take their medications due to side effects or costs. In addition, the presence of other diseases at the same time as depression can interfere with the effectiveness of antidepressants.
The article was prepared based on: